Nowadays, the medical records of every patient typically include highly sensitive information. This is especially true given that such records may contain details about a patient’s family medical history, financial situation, and other confidential data. As a result, it is crucial to safeguard and protect this information. The Health Insurance Portability and Accountability Act (HIPAA) was designed with this aim in mind. HIPAA is a federal law that outlines national standards for ensuring the privacy and security of personal health information. Compliance with HIPAA regulations is mandatory for healthcare providers, health plans, and healthcare clearinghouses to prevent costly penalties and safeguard patients’ sensitive data.
HIPAA: What is it?
HIPAA compliance is the adherence to federal regulations established by the Health Insurance Portability and Accountability Act of 1996 to safeguard the privacy and security of protected health information (PHI) by healthcare providers, health plans, and healthcare clearinghouses, as well as their business associates. The HIPAA Privacy Rule outlines guidelines for the use and disclosure of PHI, while the Security Rule establishes national standards for the security of electronic PHI. The Office for Civil Rights of the Department of Health and Human Services is in charge of enforcing HIPAA’s enforcement provisions and imposing penalties for non-compliance.
HIPAA-covered entities include:
- Healthcare providers (hospitals, clinics, doctors, dentists, optometrists, chiropractors, and psychologists)
- Healthcare clearinghouses (entities that process healthcare data for billing purposes)
- Health insurance plans (health insurance companies and government health plans such as Medicare and Medicaid)
Business associates of these entities who handle PHI on their behalf are also subject to HIPAA regulations. Business associates can include third-party service providers, such as medical billing companies, data storage companies, and lawyers.
Purpose of HIPAA compliance?
HIPAA, the Health Insurance Portability and Accountability Act, has several objectives related to healthcare privacy, security, and administrative simplification. Some of the main objectives of HIPAA include:
1. Protecting patient privacy: HIPAA establishes national standards for the protection of patients’ health information, known as protected health information (PHI). It requires healthcare providers, health plans, and other covered entities to ensure the confidentiality, integrity, and availability of PHI.
2. Ensuring the security of health information: HIPAA also requires covered entities to implement physical, technical, and administrative safeguards to protect electronic PHI (ePHI) from unauthorized access, disclosure, and destruction.
3. Facilitating administrative simplification: HIPAA aims to streamline administrative processes in the healthcare industry to reduce costs and improve efficiency. This includes standardizing electronic transactions and code sets, as well as unique identifiers for healthcare providers, health plans, and employers.
4. Reducing healthcare fraud and abuse: HIPAA includes provisions aimed at detecting and preventing healthcare fraud and abuse, including imposing penalties for fraudulent activities.
Overall, the primary goal of HIPAA is to protect patients’ privacy and ensure the security of their health information while also improving the efficiency of healthcare delivery.
What are HIPAA-compliant emails, and why are they important?
Emails sent in a way that complies with the HIPAA Privacy and Security Rules are HIPAA-compliant emails from covered entities and their business partners. These rules establish national standards for protecting the privacy and security of individual protected health information (PHI).
To ensure that emails are HIPAA-compliant, covered entities and their business associates should follow these guidelines:
- Encryption: All PHI transmitted via email must be encrypted to ensure that it is protected from unauthorized access or disclosure. Encryption helps to ensure that only authorized individuals can access the PHI, even if the email is intercepted or accessed without authorization.
- Access controls: Access to PHI transmitted via email should be restricted to authorized individuals only. Covered entities should implement access controls such as usernames and passwords to ensure that only authorized individuals can access the PHI.
- Security awareness training: Covered entities should provide security awareness training to all employees who handle PHI, including email. This training should include policies and procedures for transmitting PHI via email and how to recognize and report any potential security incidents or breaches.
- Policies and procedures: Covered entities should develop and implement policies and procedures for transmitting PHI via email. These policies and procedures need to cover things like encryption, access controls, security awareness training, and incident reporting.
- Business associate agreements: Covered entities should ensure that their business associate agreements include provisions that require business associates to comply with the HIPAA rules when transmitting PHI via email.
By following these guidelines, covered entities and their business associates can ensure that emails containing PHI are transmitted in a manner that is secure and compliant with the HIPAA rules.

What are some examples of the rules that fall under the HIPAA regulations?
HIPAA, the Health Insurance Portability and Accountability Act, includes several rules that establish national standards for the protection of individuals’ health information. The main HIPAA rules are:
- HIPAA Privacy Rule: This rule sets national standards for protecting the privacy of individual health information, known as protected health information (PHI), held by covered entities and their business associates. It requires covered entities to put in place appropriate safeguards to protect PHI and to obtain individuals’ written authorization before using or disclosing their PHI, except in certain circumstances.
- HIPAA Security Rule: This rule establishes national standards for protecting the security of electronically protected health information (ePHI) held by covered entities and their business associates. It requires the implementation of administrative, physical, and technical protections by covered entities to defend against unlawful access, use, or disclosure of ePHI.
- HIPAA Breach Notification Rule: This regulation requires covered entities to notify affected individuals, the Department of Health and Human Services (HHS), and in some cases, the media, if there is a breach of unsecured PHI.
- HIPAA Enforcement Rule: This rule establishes procedures for the investigation, enforcement, and imposition of civil money penalties for violations of the HIPAA rules. It also sets out provisions for hearings and appeals.
- HIPAA Omnibus Rule: This rule updated and strengthened many of the existing HIPAA regulations and included new provisions related to business associates and the use of PHI for marketing purposes.
Overall, the HIPAA rules work together to protect individual health information while also promoting the efficiency and effectiveness of the healthcare industry. Covered entities and their business associates are required to comply with the HIPAA rules, and failure to do so can result in significant penalties and fines.
Penalties for HIPAA violations:
The penalties for violating HIPAA can be severe, ranging from monetary fines to criminal charges. The penalties depend on the severity of the violation and the intent of the violator. The Department of Health and Human Services (HHS) has the authority to impose civil monetary penalties of up to $1.5 million per year for violations of HIPAA. In addition, the HHS Office for Civil Rights (OCR) can refer cases to the Department of Justice (DOJ) for criminal prosecution, which can result in fines, imprisonment, or both.
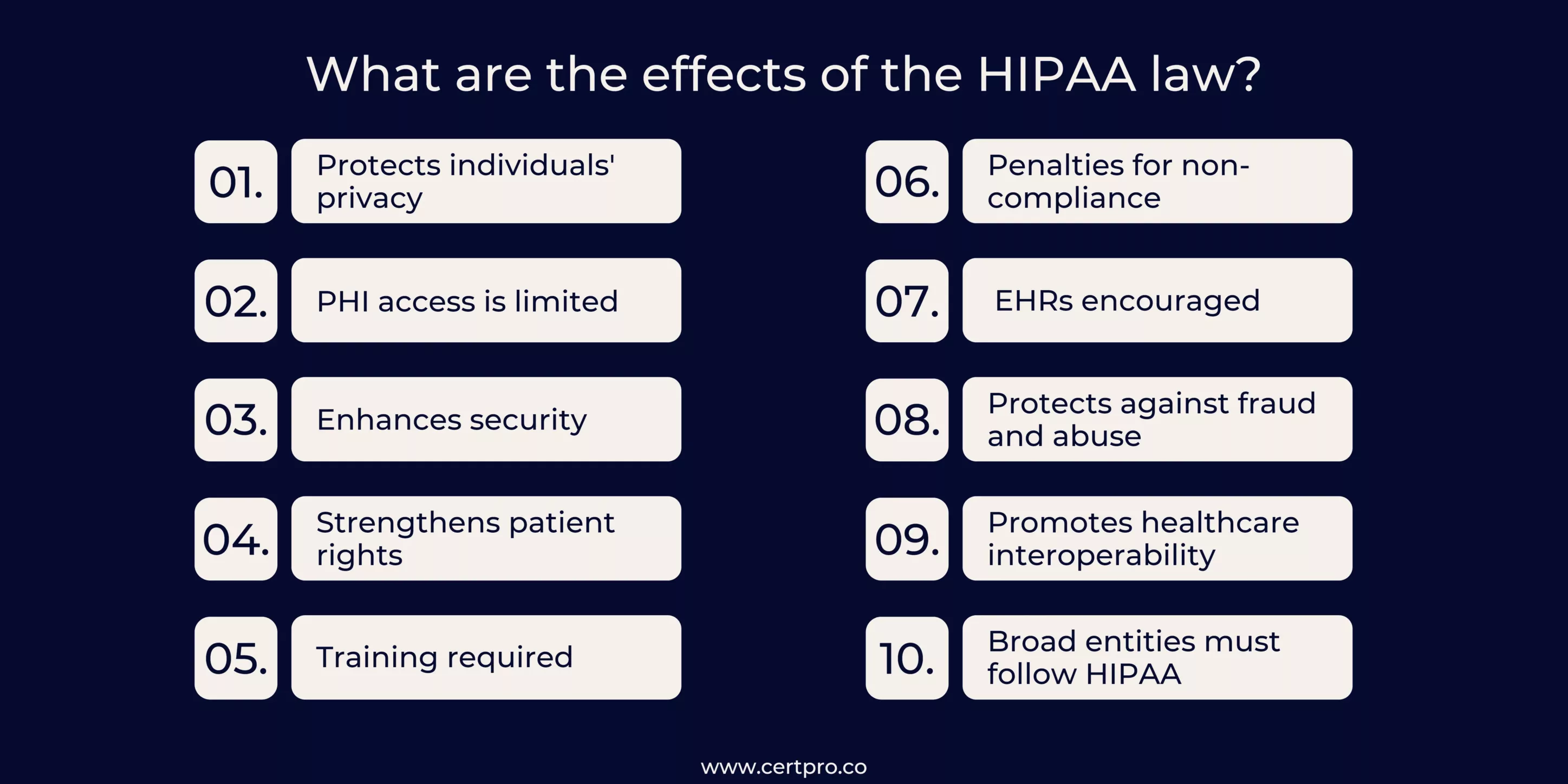
What are the effects of the HIPAA law?
- Protects individuals’ privacy: HIPAA requires healthcare providers, insurance companies, and other covered entities to protect the privacy of individuals’ health information.
- PHI access is limited; HIPAA regulates how covered entities use and disclose individuals’ PHI.
- Enhances security: HIPAA requires covered entities to implement administrative, physical, and technical safeguards to protect against unauthorized access or disclosure of electronic PHI.
- Strengthens patient rights: HIPAA gives patients the right to access their medical records, request corrections to their PHI, and restrict how their PHI is used and disclosed.
- Training required: HIPAA requires covered entities to provide training to their workforce on how to handle PHI and ensure compliance with HIPAA regulations.
- Penalties for non-compliance: HIPAA violations can result in significant penalties, including fines, civil lawsuits, and even criminal charges in some cases.
- EHRs are encouraged: HIPAA includes provisions that promote the use of EHRs, which can improve the efficiency and accuracy of healthcare.
- Protects against fraud and abuse: HIPAA helps prevent healthcare fraud and abuse by regulating how healthcare providers and insurers handle billing and payment.
- Promotes healthcare interoperability: HIPAA encourages healthcare interoperability by standardizing how healthcare data is shared and transmitted between different systems.
HIPAA Compliance with the Potential Partner
Overall, compliance with HIPAA regulations is essential for healthcare providers, health plans, healthcare clearinghouses, and their business associates to protect patients’ sensitive health information. CertPro, as a consulting company, can help organizations navigate the complex HIPAA requirements and ensure they are compliant with the law. By providing expert guidance on the HIPAA Privacy and Security Rules, CertPro can help organizations establish policies and procedures and implement appropriate safeguards to protect patients’ PHI. Ultimately, CertPro’s services can help organizations avoid potential HIPAA violations and fines while maintaining patient trust and confidence.
FAQ
What is PHI?
PHI, which stands for Protected Health Information, refers to any individually identifiable health information that a covered entity generates or receives while offering healthcare services. HIPAA regulations protect PHI in order to protect the confidentiality and privacy of patient medical information.
What are some examples of HIPAA violations?
HIPAA violations include unauthorized disclosure of patient information, failure to secure PHI, and denying patients access to their records. Examples include sharing information with unauthorized individuals, improper disposal of PHI, and using information for non-healthcare purposes. Fines and legal penalties for HIPAA violations can be significant. It’s crucial to ensure HIPAA compliance by implementing appropriate safeguards, training employees, and responding to breaches promptly.
How can I ensure HIPAA compliance?
To ensure HIPAA compliance, conduct a risk assessment, implement policies and procedures, train employees, use technical safeguards like encryption and access controls, use physical safeguards like secure storage, conduct regular audits and monitoring, and be prepared to respond to breaches.
Could covered entities legally exchange PHI with each other according to HIPAA regulations?
Yes, covered entities may legally exchange PHI with each other under HIPAA regulations, as long as they have a valid reason and comply with the minimum necessary standard for the disclosure.
Are there any exceptions to HIPAA regulations?
Yes, there are several exceptions to HIPAA regulations, including but not limited to situations involving law enforcement, public health activities, research, and national security. Additionally, some states may have additional privacy laws that provide greater protection for patient information.

About the Author
SHREYAS SHASTHA DRUPADHA
Shreyas Shastha Drupadha, a Senior Business Consultant. Serving as an ISO 27001 Lead Auditor, Shreyas ensures the establishment of robust information security management systems. His expertise also encompasses GDPR, HIPAA, CCPA, and PIPEDA implementation.
CROSS-BORDER DATA PRIVACY IN HEALTHCARE IN INDIA
Indian healthcare industries are expected to grow to approximately USD 50 billion by the end of 2025. The enormous digital innovation in healthcare sectors, remote care facilities, and artificial intelligence increase the prospects. However, the recent cyberattacks in...
DIFFERENT HIPAA REQUIREMENTS: UNDERSTANDING THE RULES AND REGULATIONS
With increasing cyberattack trends, organizations must take appropriate measures to secure their lifeblood. Similarly, patient health and financial information need protection in the healthcare sectors. Therefore, the Health Insurance Portability and Accountability...
HITECH ACT AND ITS IMPACT ON MODERN HEALTHCARE
In 2009, the Health Information Technology for Economic and Clinical Health or HITECH Act was signed to transform the American healthcare industry. The laws worked as a forward-thinking process of changing patient services. In this regard, the Patient Protection and...